Compliance Recap | January 2020
January was a busy month in the employee benefits world.
The U.S. Supreme Court (Supreme Court) denied expedited review of a court case challenging the constitutionality of the Patient Protection and Affordable Care Act (ACA). The Supreme Court also granted review of a nationwide preliminary injunction of the November 2018 contraceptive coverage exemptions final rules.
The Department of Labor (DOL) issued its annual adjustment of federal civil monetary penalties. The Department of Health and Human Services (HHS) issued its annual adjustment of civil monetary penalties.
The Centers for Medicare & Medicaid Services (CMS) released a proposed rule for benefit payment and parameters for 2021. The HHS’ Office for Civil Rights released a notice regarding enforcement of individuals’ right of access to health records under the Health Insurance Portability and Accountability Act (HIPAA) and Health Information Technology for Economic and Clinical Health Act (HITECH).
The Internal Revenue Service (IRS) released 2019 Publication 502 – Medical and Dental Expenses for use in preparing 2019 tax returns. The DOL released a new search tool for Form 5500 Filings. The DOL released a Family and Medical Leave Act (FMLA) opinion letter regarding counting employees of a health district for FMLA eligibility purposes.
Status of Court Case Challenging ACA Constitutionality
In January, the U.S. Supreme Court (Supreme Court) denied a request for expedited review of the court case challenging the constitutionality of the Patient Protection and Affordable Care Act (ACA).
As background, in 2018, 20 states filed a lawsuit asking the U.S. District for the Northern District of Texas (District Court) to strike down the ACA entirely. The lawsuit came after the U.S. Congress passed the Tax Cuts and Jobs Act of 2017 (TCJA) that reduced the individual mandate penalty to $0, starting in 2019.
On December 14, 2018, the District Court issued a declaratory order that the individual mandate is unconstitutional. The District Court found that the individual mandate is unconstitutional without the penalty and that the individual mandate is inseverable from the rest of the ACA. Because of its findings, the District Court declared that the individual mandate and the entire ACA – including its guaranteed issue and community rating provisions – are unconstitutional.
On December 18, 2019, the U.S. Court of Appeals for the Fifth Circuit (Appeals Court) held that the ACA’s individual mandate is unconstitutional. The Appeals Court is remanding the case to the District Court for additional analysis on whether the individual mandate can be severed from the ACA. The Appeals Court is also directing the District Court to consider the government’s new arguments regarding the relief that should be provided to the plaintiff states and the two individual plaintiffs in the case.
On January 3, 2020, the defendant state attorney generals and the U.S. House of Representatives asked the Supreme Court to hear an appeal of the Appeals court decision. The defendants also requested an expedited briefing schedule for the case to be heard in 2020. On January 21, 2020, the Supreme Court denied expedited review of the case. The Supreme Court has not denied the potential for a full review of the case at a later date.
Read more about the status of the court case challenging ACA constitutionality.
Supreme Court Grants Review of Contraceptive Coverage Exemptions Final Rule Case
As background, the Patient Protection and Affordable Care Act (ACA) requires that non-grandfathered group health plans and health insurance issuers offering non-grandfathered group or individual health insurance coverage provide coverage of certain specified preventive services, including contraceptive services, without cost sharing. The Treasury, Department of Labor (DOL), and Department of Health and Human Services (HHS) (collectively, the Departments) released two final rules on November 7, 2018, regarding contraceptive coverage exemptions based on religious beliefs and moral beliefs. These rules finalize the Departments’ interim final rules that were published on October 13, 2017.
On January 13, 2019, the U.S. District Court for the Northern District of California (California Court) granted a preliminary injunction that prohibits the final rules’ implementation and enforcement against the thirteen plaintiff states. On January 14, 2019, the U.S. District Court for the Eastern District of Pennsylvania (Pennsylvania Court) granted a nationwide preliminary injunction that prohibits the implementation of the two final rules. On June 5, 2019, the U.S. District Court for the Northern District of Texas (Texas Court) issued a permanent injunction against the ACA’s contraception mandate. The California Court and Pennsylvania Court preliminary injunctions were affirmed by the U.S. Court of Appeals for the 9th Circuit and the U.S. Court of Appeals for the 3rd Circuit respectively.
The plaintiff and the federal government asked the U.S. Supreme Court (Supreme Court) to hear an appeal of the 3rd Circuit decision. On January 17, 2020, the Supreme Court granted review of the 3rd Circuit decision and consolidated this case with a similar case decided by the 3rd Circuit, affirming a nationwide preliminary injunction prohibiting implementation of the two final rules.
Read more about the contraceptive coverage exemptions court cases.
DOL Releases Inflation-Adjusted Federal Civil Penalty Amounts
On January 23, 2019, the Department of Labor (DOL) issued its Federal Civil Penalties Inflation Adjustment Act Annual Adjustments for 2020 which is the DOL’s annual adjustment of federal civil monetary penalties.
Here are some of the adjustments:
- Form 5500: For failure to file, the maximum penalty increases from $2,194 to $2,233 daily for every day that the Form 5500 is late.
- Summary of Benefits and Coverage: For failure to provide, the maximum penalty increases from $1,156 to $1,176 per failure.
- Medicaid/CHIP notice: For failure to provide, the maximum penalty increases from $117 to $119 per day per employee.
- For failure to provide documents to the DOL upon its request, the maximum penalty increases to $159 per day, not to exceed $1,594 per request.
The adjustments are effective for penalties assessed after January 15, 2020, for violations occurring after November 2, 2015.
HHS Releases Inflation-Adjusted Federal Civil Penalty Amounts
The Department of Health and Human Services (HHS) issued its Annual Civil Monetary Penalties Inflation Adjustment. Here are some of the adjustments:
- Medicare Secondary Payer:
- For failure to provide information identifying situations where the group health plan is primary, the maximum penalty increases from $1,211 to $1,232 per failure.
- For an employer who offers incentives to a Medicare-eligible individual to not enroll in an employer-sponsored group health plan that would otherwise be primary, the maximum penalty increases from $9,472 to $9,639.
- For willful or repeated failure to provide requested information regarding group health plan coverage, the maximum penalty increases from $1,542 to $1,569.
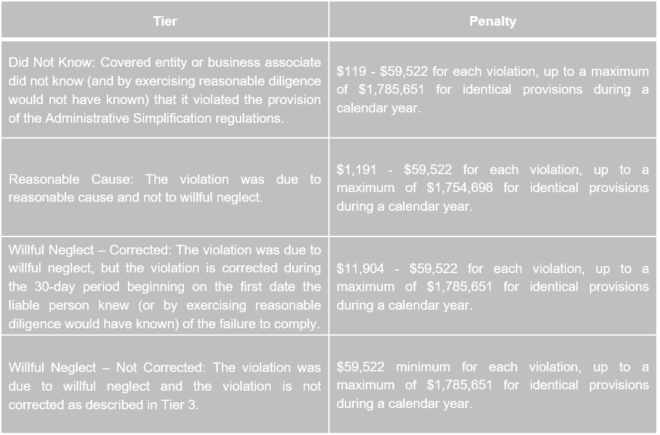
- Health Insurance Portability and Accountability Act (HIPAA):
The adjustments are effective for penalties assessed on or after January 17, 2020, for violations occurring after November 2, 2015.
Proposed 2021 Benefit Payment and Parameters Rule
The Centers for Medicare & Medicaid Services (CMS) released a proposed rule for benefit payment and parameters for 2021. CMS also released its draft 2021 actuarial value calculator and draft 2021 actuarial value calculator methodology.
Although the proposed rule would primarily affect the individual market and the Exchanges, the proposed rule addresses the following topics that may impact employer-sponsored group health plans:
- Notice requirements for excepted benefit health reimbursement arrangements (EBHRAs)
- Special enrollment period for non-calendar year qualified small employer health reimbursement arrangements (QSEHRAs)
- Maximum annual limitation on cost sharing for plan year 2021
- Cost-sharing requirements and drug manufacturers’ coupons
March 2, 2020, is the due date for public comments on the proposed rule. CMS usually finalizes its benefit payment and parameters rule in the first quarter of the year following the proposed rule’s release.
Read more about the proposed rule.
OCR Recognizes District Court Order Regarding Individuals’ Right of Access to Health Records
On January 23, 2020, the U.S. District Court for the District of Columbia (Court) vacated portions of the Health Insurance Portability and Accountability Act (HIPAA) Omnibus 2013 final rule (Final Rule) regarding the individual right of access to protected health information (PHI).
The Court held that requiring PHI to be delivered to third parties, regardless of the PHI’s format, went beyond the requirements of the Health Information Technology for Economic and Clinical Health Act (HITECH).
The Department of Health and Human Services’ Office for Civil Rights (OCR) released a notice recognizing the Court’s ruling. OCR will not enforce the requirement for covered entities to provide PHI to a third party regardless of the record’s format and will not require covered entities to charge the patient rate when providing PHI to a third party when directed by the individual to whom the PHI relates.
IRS Releases 2019 Publication 502 – Medical and Dental Expenses
The Internal Revenue Service (IRS) released 2019 Publication 502 – Medical and Dental Expenses for use in preparing 2019 tax returns.
DOL Releases New Search Tool for Form 5500 Filings
The Department of Labor (DOL) released a new search tool for Form 5500 filings. In addition to searching for specific filings, the tool allows users to search for filings using new filters including plan type, plan asset value, number of participants, employer plan types, business codes, form years, and locations. Form 5500 filings since January 2010 are available in the new search tool.
DOL Releases FMLA Opinion Letter Regarding Counting Employees of a Health District
The Department of Labor (DOL) released a Family and Medical Leave Act (FMLA) opinion letter (Opinion Letter) on whether a health district must count the employees of the county in which the health district is located for purposes of determining FMLA eligibility for its employees. The DOL notes that, under the FMLA, a state or political subdivision of a state constitutes a single public entity for determining employee eligibility. Whether two agencies of the same state or local government constitute a single public entity must be determined on a case-by-case basis.
The Opinion Letter provides a non-exhaustive list of eight factors to consider when determining whether a public entity is a single entity for FMLA purposes, including whether the two agencies have separate payroll systems and whether they have separate hiring and other employment practices.
Question of the Month
- When the plan changes, when should I give notice to participants?
- Depending on the change that is made, an employer must provide notice within one of three time frames:
- 60 days prior to the change
- No later than 60 days after the change (or, within 60 days of the change)
- Within 210 days after the end of the plan year
For modifications to the summary plan description (SPD) that constitute a material reduction in covered services or benefits, notice is required within 60 days of adoption of the material reduction in group health plan services or benefits. For example, a decrease in employer contribution would be a material reduction in covered services or benefits so notice should be provided within 60 days of the change in employer contribution. As a best practice, an employer should give advance notice of the change. For practical purposes, employees should be told prior to the first increased withholding.
If a plan makes a material modification in any of the plan terms that would affect the content of the most recently provided summary of benefits and coverage (SBC), then notice must be provided no later than 60 days prior to the date on which the modification will become effective.
However, if the change is part of open enrollment, assuming you communicate the change during open enrollment, the open enrollment communication is considered acceptable notice, regardless of whether the SBC or the SPD, or both, are changing. Open enrollment is essentially a safe harbor for the 60-day prior/60-day post notice requirements.
Finally, changes that do not require more immediate notifications, because they do not affect the SBC and are not a material reduction in benefits, must be communicated through a summary of material modifications or an updated summary plan description within 210 days after the end of the plan year.
2/3/2020