Compliance Recap | September 2021
September saw a lot of activity in the compliance space, especially coming from the federal government.
Vaccine Mandate Guidance Still Pending
Vaccine mandates were on everyone’s mind, especially after Delta Airlines announced its $200 monthly surcharge and weekly testing program for unvaccinated employees. The government joined the fray when President Biden released his Path Out of the Pandemic, a national strategy to combat the spread of COVID-19 variants. It included a series of executive orders requiring federal employees and contractors to get vaccinated, as well as directing the Occupational Safety and Health Administration (OSHA) to draft an emergency rule requiring businesses with 100 or more employees to ensure their workers are vaccinated or submit to weekly testing. Until OSHA releases its emergency temporary standard, employers are left questioning what can and cannot be done to prepare. UBA and Fisher Phillips released a Compliance Advisor on this special topic.
IRS Releases Guidance on Sick Leave and Qualified Family Leave Reporting
The IRS released Notice 2021-53, which gives technical guidance to employers on the requirement to report qualified sick leave wages and qualified family leave wages paid to employees in 2021 under the Families First Coronavirus Response Act and the Internal Revenue Code.
COBRA Subsidy Expiration Notices Due
There was a flurry of activity to get the American Rescue Plan Act COBRA subsidy expiration notices out by September 15 for those assistance-eligible individuals whose COBRA premium subsidy was to end on September 30, 2021. The Department of Labor provided a model expiration notice with instructions.
Departments Issue Proposed Rules Regarding No Surprises Act
The Departments of Health and Human Services, Labor, and Treasury (the Departments), along with the Office of Personnel Management (OPM), released a notice of proposed rulemaking regarding the No Surprises Act. The proposed rules relate to air ambulance services reporting requirements, agent and broker disclosures for individual health insurance coverage and short-term limited duration insurance, and new procedures for enforcement of Public Health Service Act provisions. Comments are to be received by October 18, 2021, to be considered. The Departments and OPM also released an interim final rule under the No Surprises Act explaining the independent dispute resolution process. Read the UBA/Fisher Phillips Compliance Advisor for more information.
Revisions Proposed to Form 5500 Annual Report
The Departments of Labor and Treasury, and the Pension Benefit Guaranty Corporation released a notice of proposed revisions to the Form 5500 Annual Report and a notice of regulatory changes to the applicable Form 5500 regulations under Title I of ERISA. Although intended to implement provisions of the SECURE Act, the proposed changes will also add reporting requirements for multiple employer welfare arrangements (MEWAs) in the Form M-1. The agencies are asking for comments on the proposed revisions to be submitted no later than November 1, 2021. If the proposed changes are adopted, they would generally apply to plan years beginning on or after January 1, 2022. For more information, see the Department of Labor’s news release.
CMS Finalizes 2022 Benefit and Payment Parameters
The Centers for Medicare & Medicaid Services (CMS) finalized rules proposed earlier this year amending various benefit and payment parameters and other Affordable Care Act (ACA) and exchange-related rules. The rules will expand the federal exchange enrollment period starting with the 2022 coverage year – November 1 through January 15. It also adopts the proposed monthly exchange special enrollment period for certain individuals. Importantly, the rules finalize a technical amendment to the ACA essential health benefits requirements, clarifying that health plans required to cover essential health benefits must be comply with Mental Health Parity and Addiction Equity Act. Although these changes are mainly for insurers and exchanges, plan sponsors and advisors are advised to review the proposed rules for any potential consequences to their own plans. For more information, see the text of the rule and the CMS fact sheet.
IRS Releases Draft ACA Reporting Forms for 2021
The IRS released draft ACA reporting forms and instructions for 2021: draft Forms 1094-B, 1095-B, 1094- C, 1095-C, as well as instructions for draft B and draft C. Notably, draft Form 1095-C and instructions included two new codes to report affordable ICHRA coverage. Keep in mind, these are drafts and are subject to further change before final release.
CMS Releases 2022 Premiums and Cost-Sharing for Medicare Advantage and Part D Plans
CMS released the 2022 premiums, deductibles, and other important information for Medicare Advantage and Part D plans. In the press release, CMS announced that the average Medicare Advantage premium will be $19 per month and average Part D premiums will be $33 per month. The press release also contains links to related CMS resources.
IRS Announces 2022 ACA Affordability Requirement
The IRS announced that the ACA affordability requirement will be met for 2022 if the lowest-cost, self- only coverage option does not exceed 9.61% of an employee’s income. This adjustment, found in Revenue Procedure 2021-36, is down from 9.83% in 2021. For employers using the federal poverty line safe harbor, employee-only coverage should cost no more than $103.14 per month. Care should be taken that plans adjust for this change, especially as costs are expected to increase in 2022.
Departments Issue Guidance on Transparency in Coverage Rules
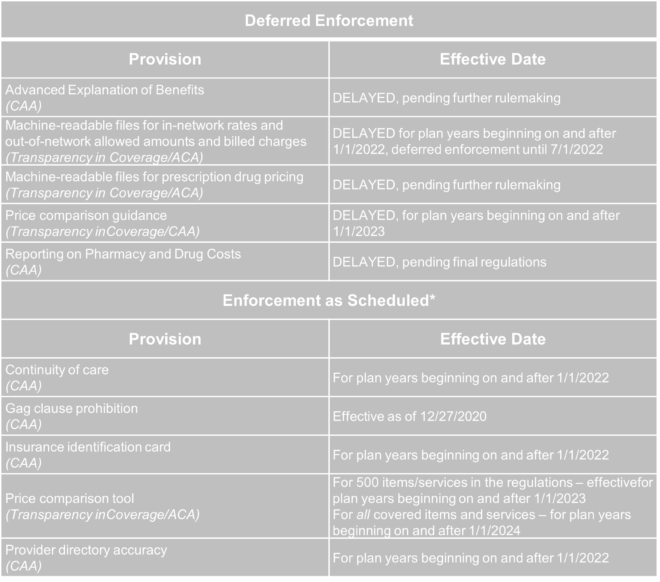
The Departments of Health and Human Services, Labor and Treasury issued FAQ guidance to group health plans and health insurance carriers to aid in compliance with the final Transparency in Coverage Rules issued under the Affordable Care Act (ACA) and Consolidated Appropriations Act (CAA). This guidance, issued August 20, 2021, also delayed the effective date of several of the provisions, though not all. UBA and Fisher Phillips issued a Compliance Advisor to discuss the guidance – see “Departments Defer Transparency and Disclosure Rule Enforcement, Provide FAQ Guidance” for details.
For a quick breakdown of which provisions will be subject to delayed enforcement and which provisions will be enforced, review the following chart.
* Plans are to use good faith, reasonable efforts to comply until further guidance issued.